Health behaviour change: a place-based solution
In December 2021, the NHS in England experienced its worst A&E waiting times since records began, with around 13,000 patients waiting more than 12 hours to be seen. In the same month, more than three-quarters of a million people waited more than four weeks to see their GP after making an appointment.
With these ongoing impacts of the pandemic on the general wellbeing of the population, and on NHS staffing levels, it’s rarely been more important to reduce pressure on healthcare services. A key strategy for achieving this is to help patients choose the right service for their needs, including self-care, where appropriate.
Informed choices
With this goal in mind, we are working with NHS Mid and South Essex Integrated Care System to develop a system-wide behaviour change campaign to ensure parents and carers of children aged 0-5 make informed choices about where to access the right advice and support for common childhood illnesses.
We worked with the client to define key goals, including:
- Increase the number of parents and carers of 0-5-year-olds who access and use self-care tools (such as the client’s app) to treat common childhood illness.
- Reduce the number of parents and carers of 0-5-year-olds attending the GP or A&E with symptoms that could be treated at home.
- Reduce the number of parents and carers of 0-5s making repeat visits to the GP with common childhood illnesses.
Our list of priority audiences included:
- Parents and carers of 0-5-year olds (family, nurseries, early years settings etc.).
- Healthcare professionals (midwives, health visitors, nursery and school nurses, GPs etc.).
- Partners (children’s and family centres, mum and baby groups, soft play centres, retailers etc.).
Invaluable insights
We began with desk research and insight gathering, including on the frequency of GP attendances of 0-5-year-olds in target areas. We then held co-creation workshops with parents, carers and healthcare professionals (HCPs) to explore a range of factors, including: usage of and trust in NHS websites; interest in app-based solutions and other channels; and preferences on brand, messaging and information structure.
The insights from this process were invaluable, including:
- All parents felt that direct engagement through the community was the best way of getting information to them, including through: early years settings, nurseries, libraries, community centres, faith groups, breastfeeding support networks, etc.
- Many did not engage with traditional media, with some using social media extensively – hence digital resources, such as a website and an app were expected.
- Simplified, chunked-down, and highly-visual information was essential, with the need for clear positioning of services, in a way that audiences from all backgrounds could understand.
From this insight we made some immediate recommendations, including developing urgent self-care at home guidance, to be delivered via print, digital and social media channels. And we created companion materials for HCPs and others to use in community settings, and at weigh-ins and health checks etc.
The content, tone and look and feel of these communications was carefully calibrated in response to the input and insight from parents and carers. You can see extracts of the various print and digital outputs below.
Place-based change
With phase one of the work well underway, we then asked how we might go further in the upcoming phase two, to truly embed these behaviours in the community.
Our approach is to look to apply the population intervention triangle for place-based behaviour change from PHE’s Reducing health inequalities: system, scale and sustainability1. In the words of the report: “Developing integrated place-based systems is key to ensuring the long-term sustainability of health and care services. Strategies that are multifaceted and complementary are more likely to bring success.”
Three key facets of joined-up strategies are indicated in the Population Integration Triangle, below:
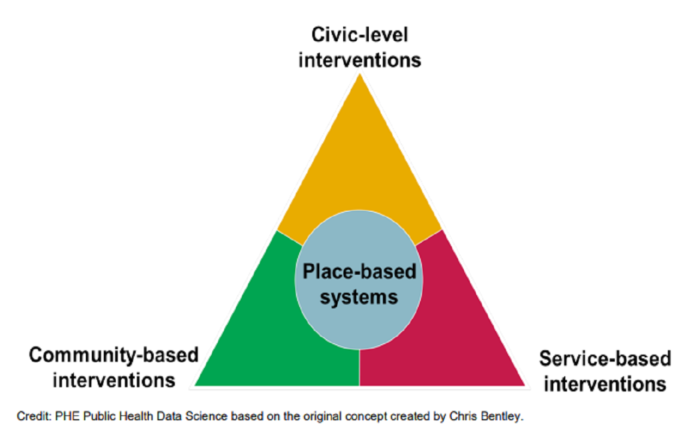
Each component of the triangle dovetails neatly with the others, and is likely to be more effective as a result, where:
- Civic level interventions are public policy change to drive the social determinants of health and make healthy choices easier.
- Community based interventions involve engaging groups of common interest, building social and peer support networks etc.
- Service-based interventions means accessible, high-quality services that produce good outcomes for individuals (while scaling to the population level).
Based on this tried and tested model, our recommended implementation for phase two includes:
- Creating a child-health expert role based in the community.
- Working with GP practices to develop a process to identify and directly support ‘frequent visitors’ from the target audience.
- A partner communications and engagement plan – including a toolkit and regular ezine – to support ongoing collaboration.
- Developing training materials to help ‘train the trainer’ – such as guides, infographics, and a webinar or overview video.
- Considering programmes of work with employers – particularly healthcare providers or others in the public sector – to model family-friendly healthcare policies.
Learn more
The anticipation is that this insight-led creative intervention, and underpinning place-based strategy, will help drive behaviour change amongst local parents and carers of 0-5-year-olds, and help ease some of the strain on local care services during this period of unprecedented demand.
To learn more about place-based behaviour change, or to discuss any of your challenges around making healthier choices easier, please contact me at Amy.Burgess@Corporateculture.co.uk
Sources: